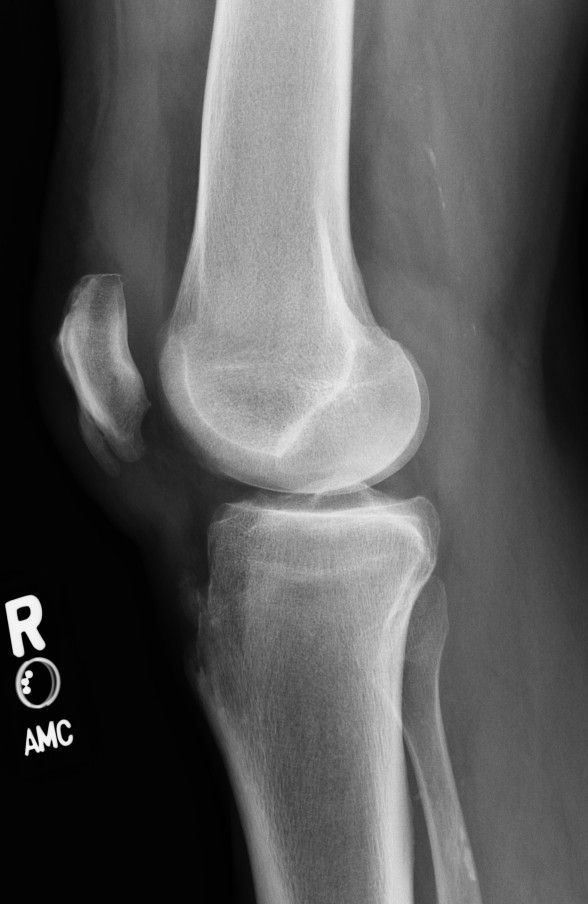
Season 10 Case 11
History: Knee Pain
Do any names come to mind? Are the findings related to the patient's current pain?


Answer:
CLICK HERE FOR ANSWER
Answer:
1) Sequela of prior Osgood-Schlatter's disease
2) Sequela of prior Sinding-Larsen-Johansson disease
Osgood-Schlatter's disease
- a fatigue or traction injury of the distal patellar tendon at it's insertion on the tibial tubercle
- usually due to recurrent microtrauma
- classically affects boys 10-15 years old (particularly those with frequent jumping or kicking)
At presentation there is focal pain at the tibial tubercle. Presentation is almost always pathognomonic so imaging is not often performed.
Radiographs can show focal soft tissue swelling over the tibial tubercle. After about 3-4 wks of healing is when the classic small ossifications/ fragmentations develop, which can persists indefinitely.
MRI of acute disease shows a thickened, edematous distal patellar tendon with pre-tibial soft tissue edema. +/- underlying bone edema or associated infrapatellar bursitis.
Treatment is conservative with rest, ice, limiting activity and antiinflammatory medicines.
Sinding-Larsen-Johansson disease
- essentially the same pathology as above but affecting the patellar tendon origin from the inferior patella
- again, classically affects boys 10-14 years old (also associated with jumping/kicking)
Presentation is focal pain/swelling at the inferior pole of the patella, and again is fairly pathognomonic in this age group (very similar to the pathology of "Jumper's knee" which is seen at all ages).
Radiographs can show focal soft tissues swelling over the inferior pole of the patella. Sometimes one is able to make out thickening of the proximal patellar tendon with stranding anterior and/or posterior to the tendon. Over time you can get fragmentation/small ossification of the proximal tendon (similar to Osgood-Schlatter's), or enthesophyte formation.
MRI/US of acute disease will show thickening and edema within the proximal patellar tendon +/- inferior patellar bone edema.
Again, treatment is conservative with rest, ice, limiting activity and antiinflammatory medicines.
Our case

The green arrow shows the sequela of Sinding-Larsen-Johansson, ie fragmentation/enthesopathy formation of the lower pole of the patella.
The blue arrow shows sequela of Osgood-Schlatter's disease with fragmentation/ossification in the distal patellar tendon.
Note that there is no significant soft tissue swelling at either site. Additionally it is pretty obvious that this patient has fused growth plates which puts them out of the realm for either of these syndromes. So these changes are NOT ACUTE. Rather, they presumably had both syndromes as an adolescent and these are the benign changes that persisted.
The key to remember is that these changes are not those of acute disease, rather, as makes sense, the calcification is a typical part of the healing process. Similar processes take place at:
- triceps tendon insertion on the olecranon
- biceps tendon insertion on the radial tuberosity
- Achilles tendon insertion on the posterior calcaneous
- plantar fascia origin of the inferior calcaneous
So if you mention them for an adult, make sure you specify that these are remote or chronic findings.
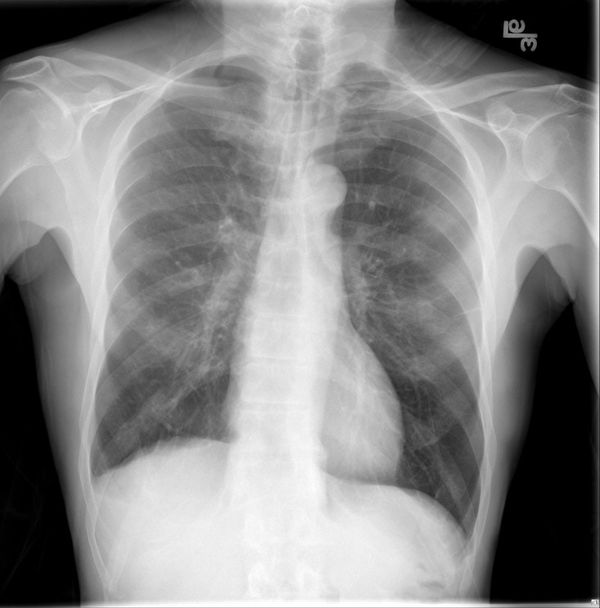
Just of interest, would you like to see the contralateral side?