Season 10 Case 12
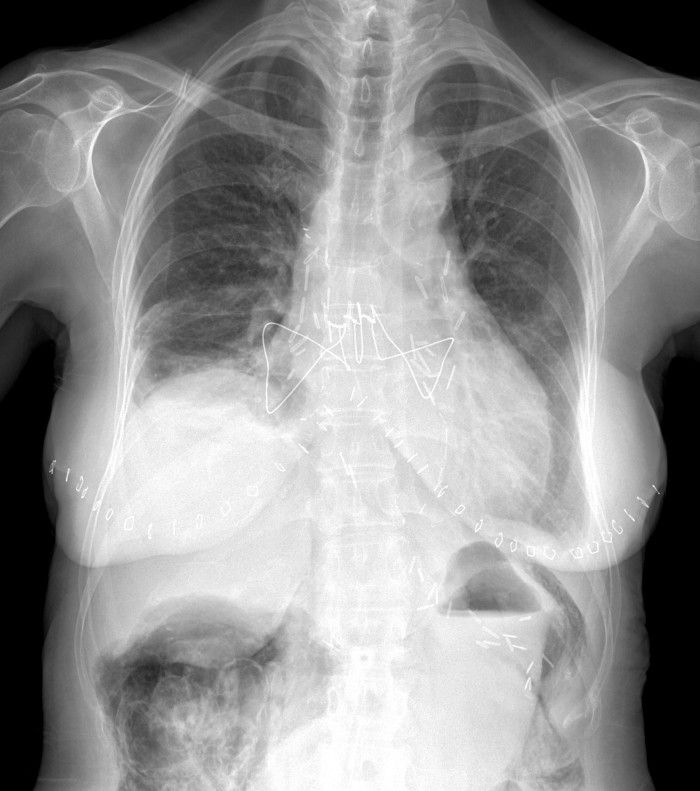
History: 2 week follow-up post surgery. What is the important finding? Can you tell what type of surgery this patient underwent?

Answer:
CLICK HERE FOR ANSWER
Answer: Pneumatosis coli status post bilateral orthotopic lung transplant (BOLT)
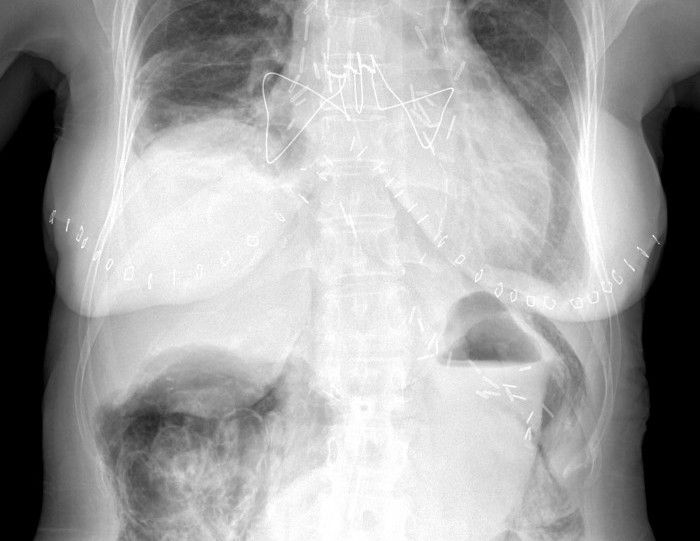
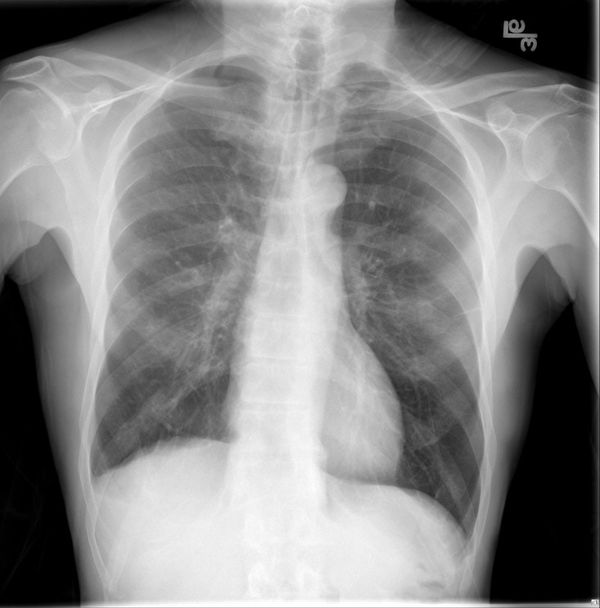
While the specific surgery may or may not be important (we'll get to that later), you can clearly see the surgical clips over both hilar regions, the extensive mediastinal wires and the bilateral cutaneous staples. This is consistent with a bilateral lung transplant.
More importantly, did you see the finding in the abdomen?
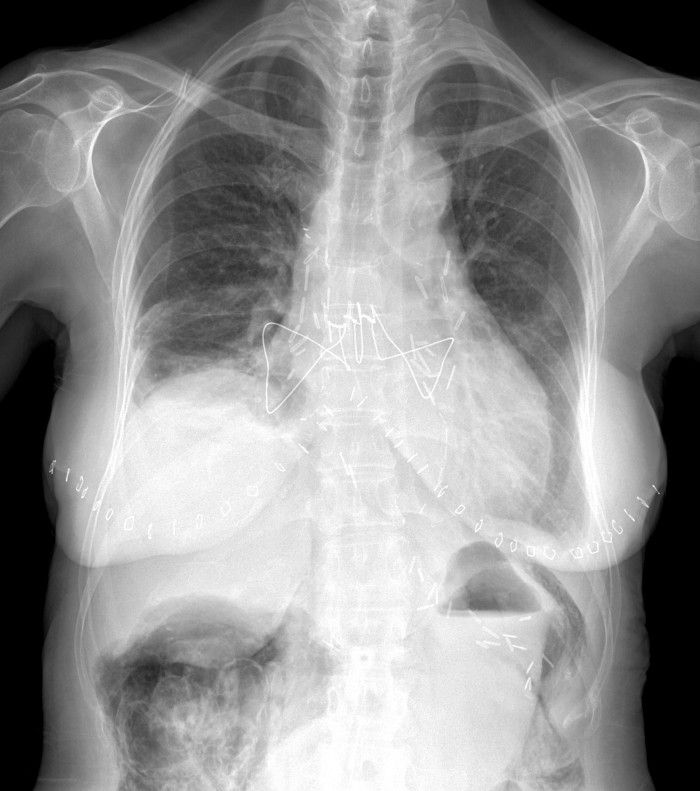

There is extensive air/pneumatosis involving the colon. While the abdominal view does a good job showing the extensive gas in the wall of the ascending colon, the upright chest X-ray demonstrates it well in the splenic flexure.
Want a better look?

Pneumatosis coli
Pneumatosis coli is the term used to describe the appearance of intramural gas within the colonic wall. When it is the small bowel that is involved it is termed pneumatosis intestinalis. When it has a more cystic appearance, the term cystoides can be added to either version.
Pathologic composition of the gas depends on the etiology.
Etiology
Divided into 2 groups:
Benign:
- Pulmonary disease (asthma, emphysema, cystic fibrosis, etc)
- iatrogenic/procedural (ex jejunostomy tube placement, endoscopy)
- systemic diseases (lupus, scleroderma, AIDS)
- medications (corticosteroids, chemotherapy, lactulose)
- organ transplantation
- Primary pneumatosis- idiopathic, generally involves the colon with cystic air collections (= penumatosis cystoides coli/intestinalis)
Life-threatening:
- Intestinal ischemia
- intestinal obstruction (esp strangulation)
- enteritis/colitis (ex necrotizing enterocolitis in newborns)
- toxic megacolon
- trauma
- organ transplantation (particularly bone marrow transplant and graft-versus-host disease)
Treatment
- Depends on underlying etiology
- Correlate for any pertinent history (above) and with clinical status - ie pain, surgical abdomen
- For benign causes, simple gut rest can be sufficient
- Lab values can be helpful (serum lactate)
- CT can be very helpful to look for life-threatening etiologies, ie
- bowel wall thickening or abnormal enhancement (bad)
- more linear air collections tend to be more concerning
- portal venous gas (very bad)
- mesenteric arterial/venous thrombosis (bad)
Complications:
- Pneumoperitoneum can occur from rupture into the peritoneal cavity. Treatment still is generally based upon the causative etiology.
Our Patient:
As you've probably put together by now, this patient had undergone a bilateral orthotopic lung transplant and this was chest X-ray was performed as part of their routine follow-up. We noted above that organ transplantation is one of the known causes of benign pneumatosis coli and it seems lung transplants are a relatively common example. The vast majority of these patients seem to be of the benign type and do well with gut rest and sometimes steroids (which ironically is the major drug induced cause), but CMV colitis can be a common opportunistic infection in lung transplant recipients so consideration for antivirals may be warranted.
Our patient did fine with monitoring and had no real symptoms or issues with it improving over the next few days.
References:
- Ho LM, Paulson EK, Thompson WM. Pneumatosis intestinalis in the adult: benign to life-threatening causes. AJR Am J Roentgenol. 2007 Jun;188(6):1604-13. doi: 10.2214/AJR.06.1309. PMID: 17515383. https://www.ajronline.org/doi/pdf/10.2214/AJR.06.1309
- Chandola R, Laing B, Lien D, Mullen J. Pneumatosis Intestinalis and Its Association With Lung Transplant: Alberta Experience. Exp Clin Transplant. 2018 Feb;16(1):75-80. doi: 10.6002/ect.2016.0289. Epub 2017 Oct 31. PMID: 29108518. https://pubmed.ncbi.nlm.nih.gov/29108518/