Season 10 Case 16
History: Trauma. Abdominal pain.
Do you see anything? Any other imaging requested?

Would you like more images?
There was no free fluid within the abdomen and the rest of the abdominal structures were normal. How does this affect your impression?
Answer:
CLICK HERE FOR ANSWER
Focal Nodular Hyperplasia (FNH)
Did you know that the liver is the only self-regenerating internal organ in the human body?
Focal nodular hyperplasia is a result of this regenerative capacity, where there is proliferation of hepatocytes with abnormal vascular supply, vascular drainage and biliary drainage. This response is believed to be secondary to areas of hypo- or hyperperfusion, and thus current thought is that the presence of underlying arterial malformations can play a major role in development (note the increased incidence of FNH with Osler-Weber-Rendu syndrome (hereditary hemorrhagic telangiectasia as well as with hepatic hemangiomas). Arterial supply is generally from the hepatic artery and venous drainge is through the hepatic vein (ie NO portal venous connection).
- FNH is a benign condition, and is the second most common benign hepatic lesion behind hepatic hemagiomas
- Most commonly found in young to middle-aged adults
- 5-6x's more common in females
- Solitary most common but 20% multifocal
- 25% seen with other vascular pathologies such as hemangiomas, AVMs, Budd-Chiari syndrome (hepatic venous obstruction), portal shunts, Osler-Weber-Rendu, etc
Types:
-
Typical
- poorly encapsulated large mass (4-8cm)
- prominent central scar with radiating fibrous septae (~50% of cases) forming a pseudocapsule***
- prominent central artery with spoke-wheel configuration
- abnormal cellular architecture but can contain bile ducts and Kupffer cells (reitculoendothelial hepatic macrophages)
-
Atypical
- lacks central scar and central artery (makes diagnosis difficult)
- lacks central scar and central artery (makes diagnosis difficult)
Radiology
Ultrasound:
- variable echogenicity of both the lesion and central scar
- may be isoechoic to hepatic parenchyma and thus not seen
- sometimes can see the spoke-wheel vascularity
Multiphasic CT:
-
Non-contrast: hypo- or iso-attenuating (or hyper attenuating in a low density fatty liver)
-
Arterial: bright homogeneous arterial enhancement EXCEPT central scar
Portal Venous: washout yielding iso-hypoenhancing to liver (often difficult to even see) -
Delayed: central scar can demonstrate delayed ehancement (80%)
-
macroscopic fat, calcification and hemorrhage are not typical findings
MRI:
- T1: iso- to moderate hypointense, hypointense scar
- T2: iso- to hyperintense, HYPERintense scar
- T1 +c (Gd): intense early arterial enhancement, washout to isointense portal venous phase, persistent enhancement of scar on delayed phase
Alternate contrast agents: - Eovist/Primovist: washout is less than Gd so mild enhancement persists on delayed imaging (vs adenomas which are hypointense on delayed sequences)
- SPIO: a reticuloendothelial agent, ie taken up by Kupffer cells (see nuclear medicine below) -> hypointensity due to suscpetibility signal loss (again vs adenomas which have less to no Kupffer cells)
Nuclear Medicine:
Tc-99m Sulfur colloid is the classic radiotracer used for diagnosis. Similar to SPIO above, sulfur colloid is taken up by the reticuloendothelial system, ie the Kupffer cells, and thus it can distinguish FNH from other lesions that do not contain normal parenchymal elements. Classically FNH is "hot" (Hincreased radiotracer uptake) versus other lesions which should be "cold" (photopenic or low uptake) within the normal low level normal hepatic uptake.
Tc-99m HIDA exam should show the same uptake as normal liver. Since HIDA is taken up by hepatocytes and excreted in the biliary system, and FNH contains all the normal cells and bile ducts, it should appear background to "hot" just like the contrast agents above.
Our Patient
I presented the case a bit backwards for teaching purposes.
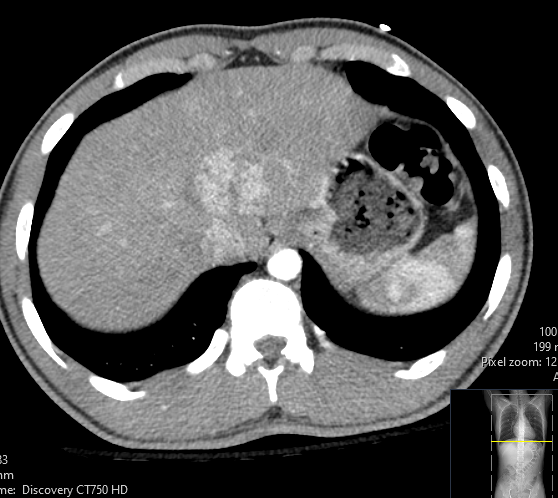
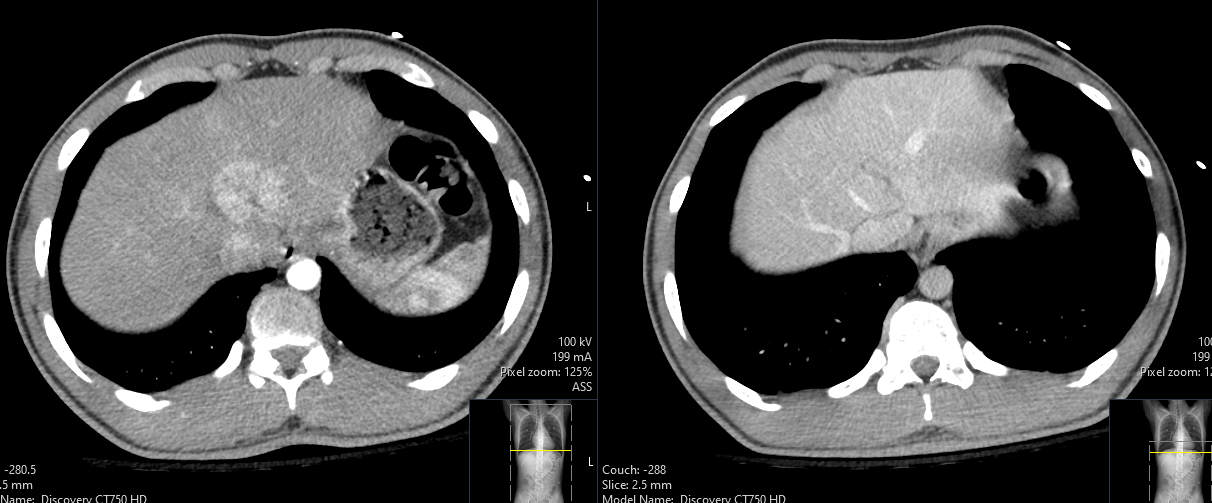
On the left we have the arterial phase. Note the rounded area of early enhancement anterior to the IVC, even showing a linear, low density central scar.
On the right we have the portal venous phase. Here we can see the normalization of the enhancement so it now is the same as the remaining liver, but we can still make out that linear, low density central scar.
Given the way I presented it and the history of trauma (which was the real history), laceration should definitely been up there on the differential. But given the arterial imaging, and lack of secondary traumatic findings, the appearance is most consitent with benign focal nodular hyperplasia




