Season 10 Case 17
History: Hand/Wrist Pain

Answer:
CLICK HERE FOR ANSWER
Rheumatoid Arthritis (Wrist)
Rheumatoid arthritis is a chronic autoimmune inflammatory disorder that affects numerous organs, the most classic of which are joints and synovial soft tissues.
- overal prevalence of ~1% of the population
- onset typically in 4th- 5th decade of life
- 2-3x's more common in females
It is theorized that through a combination of genetic predisposition (HLA-DR B1 allele) and some environmental trigger (Ebstein-Barr virus is thought to play a role), the body initiates an autoimmune response. IL4, TNF, and B-cells produce Rheumatoid Factor antibodies against natural IgG yielding immune complexes that are deposited through the body. This response attacks numerous organ systems such as the skin, heart, lungs, and classically the joints of the musculoskeletal system.
For this brief write-up, I am going to focus primarily on the articular manifestations of RA.
- Inflammation -> pannus formation (ie thickened, hyperplastic synovium)
- Pannus contains granulaton tissue including lymphyocytes, plasmacytes, macrophages and osteoclasts
- The pannus slowly destroys the articular cartilage, however the "bare areas", which are the small areas of exposed bone peripheral to the cartliage but still contained within the joint space (see image below), are less protected than the cartilage and show destructive changes much earlier.

Clinical Presentation (MSK):
- Onset can be slow or rapid
- Inflammatory appearance: warm, painful, swollen and stiff joints with limited range of motion
Radiology
Radiography:
- Marginal erosions - ie at the "bare areas" we described above (it seems to favor the radial side of the metacarpophalangeal joints). As it progresses, the pannus/inflammation evidentually errodes through the articular cartilage to get more diffuse erosions and subchondral cyst formation (fluid extending into the bone through areas of articular/cortical destruction)
- Joint space loss - typically concentric and symmetrical
- Osteoporosis - inflammation yields hyperemia about the joints -> increased bone resorption in a periarticular distribution
- Soft tissue swelling - inflammation -> edema about the involved joints
Hand/Wrist Specifics:
- RA involves the more proximal joints of the wrist and hand such as the intercarpal, MCP (especially 2nd and 3rd), and PIP joints and typically spares the DIP joints
- Ulnar styloid is a classic site of erosion in RA
- Late Stage changes:
- carpal instability and SLAC wrist (scapholunate advanced collapse)
- hitchiker's thumb deformity (flexion of 1st MCP and hyperextension of 1st PIP joint)
- joint anylosis
- joint subluxation (ulnar deviation at MCP joints, boutonniere deformity and swan-neck deformity)
- pencil-in-cup deformity (classically taught as characteristic of psoriatic arthritis, it also commonly occurs in RA)
- scallop sign (erosion of the radius at the distal radial ulnar joint - though to prelude extensor tendon rupture)
Other Imaging Modalities
Ultrasound
- Ultrasound can be an early diagnostic tool in articular assessment of RA by examining the synovium itself. Even before bone destruction you can see:
- synovial thickening/hypertrophy
- synovial hyperemia
- bursitis
- tenosynovitis - ie fluid and inflammation involving the tendon sheath (classic is the extensor carpi ulnaris tendon)
And Ultrasound can even be useful for interarticular steroid injectons as treatment.
MRI
- MRI is very sensitive to similar findings above
- synovial thickening (shedding of pieces of synovium -> rice bodies)
- synovial hyperemia
- pannus formation
- subchondral edema, csyts and erosions
- cartliage thinning/destruction
as well as:
- joint effusions
- periarticular marrow edema (ie osteoclastic activity and osteopenia)
Summary (TLDR)
- Rheumatoid is an INFLAMMATORY process affecting joints
- Clinical symptoms of inflammation (swelling, redness, pain)
- Pannus affects "bare areas" so periarticular erosions/destruction (note the lack of productive change till superimposed osteoarthritis develops
- Wrist is classic joint for involvement, affecting the proximal joints (intercarpal, MCP, PIP) versus OA being more wear phenomenon affecting distal joints
- Classic ares of involement:
- ulnar styloid erosions
- 2nd and 3rd MCP joint erosions
- triquetral erosions
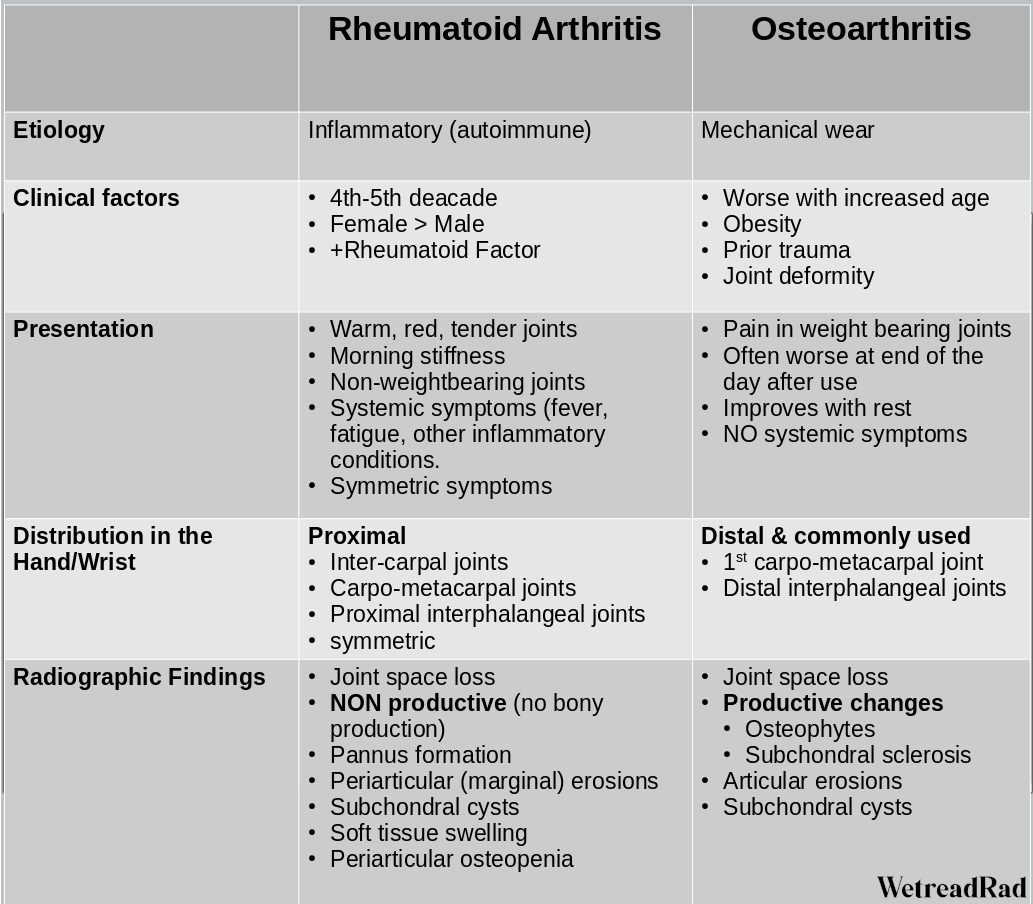
A common problem is that everyone seems to want to call everything "degenerative", ie osteoarthritis. As we've already stated, osteoarthritis is a mechanical wear phenomenon. Essentially the cartliage just wears down. Since bone doesn't particularly like to rub against other bone, and really the only thing bone can do is make more bone, it uses productive processes to reinforce the cortex (subchondral sclerosis) while bridging the joint to minimize further wear (osteophytes limiting joint motion).
If you are confusedm, here is a table I made up to help differentiate between the two:
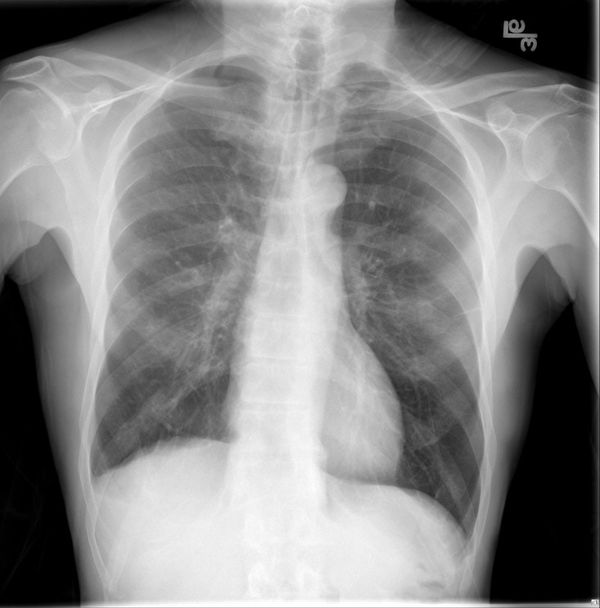
Our Patient



Here we have a 61 yo female with 2 months of worsing atraumatic wrist and hand pain.



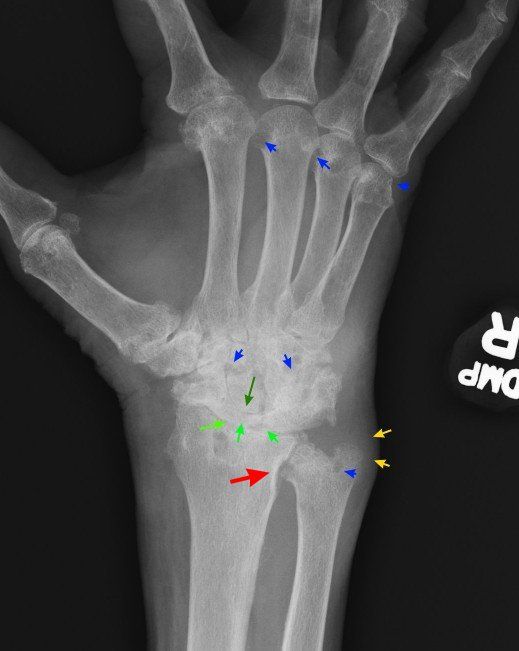
Radiographic Findings:
- Diffuse intercarpal joint space loss and carpal/ulnar styloid erosions (blue arrows). Note the large subchondral cyst in the distal radius (long blue arrow)
- radiocarpal joint space loss (light green arrows) with proximal migration of the capitate (dark green arrow) consistent with developing SLAC wrist
- scalloping of the radial aspect of the Distal radial ulnar joint (red arrow)
- soft tissue swelling over the ulnar styloid consistent with tenosynovisits of the extensor carpi ulnaris tendon (yellow arrows)